My Errant Uterus

I keep my uterus on the bottom shelf of my dresser.
It is cool and dark there, suitable for a preserved organ. Before my hysterectomy in 2019, I kept it in its original container, my pelvis. For most of my lifetime, since before my birth, it nested softly in the company of my ovaries, fallopian tubes, bladder, and rectum. In my teen years, it shed blood and tissue monthly, and much later, cradled my daughters as they were developing fetuses. It was opened with a scalpel during my cesarean sections in 2001 and 2004. The first operation was an emergency, the second a surrender after 36 hours of labor.
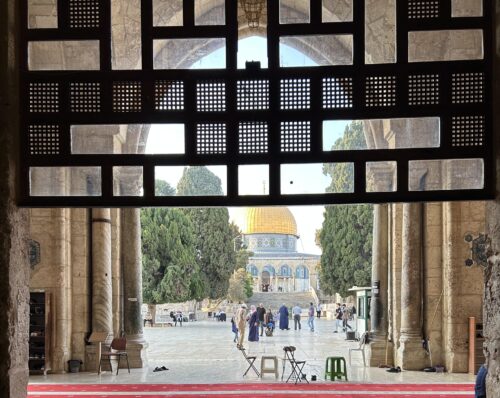
My uterus is an adventurous spirit, traveling to places even I have not visited. Now it floats in a pool of formaldehyde in a white plastic container next to my gym clothes.
Before telling you how my uterus ended up outside of my body, let me tell you how being a person born with a uterus has shaped my life experiences.
I was gendered female at birth and raised as such in the United States. I identify as a woman, and this is important for the story I tell and the ways that my body has been viewed and treated by health care professionals. I am a mother to two young adult daughters, and I am also a woman who has terminated two pregnancies. The first was at age 19 after a diaphragm malfunction and the second was in my late 20s, during an emotionally abusive relationship unsuitable for progeny.
I am also a sociologist and bioethicist of health, illness, bodies, reproduction, gender-based violence, and trauma. I have written books and articles on fetal surgery, reproductive technologies, infant mortality, maternal health, breast and cervical cancers, environmental toxins, and more.
I am a women’s health expert, in more ways than one.
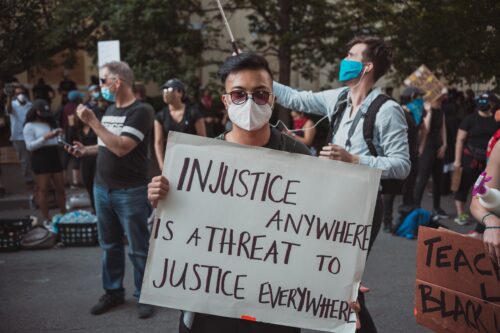
Several recent books have explored the mysteries of the womb, revealing health scientists still do not know much about how uteruses work. Yet this has not prevented politicians, judges, and others from discussing them in congressional chambers, courtrooms, and the media. At issue for many such “authorities” is who owns the uterus. Or, rather, who owns the contents—most specifically, embryos and fetuses—of a pregnant uterus.
The answer to who owns the uterus might seem obvious, given that uteruses are located inside people’s bodies. Yet, surprisingly, their ownership is contested.
Reproductive politics, especially abortion, have dominated public discourse for decades in the U.S. The U.S. Supreme Court’s 2022 ruling in Dobbs v. Jackson Women’s Health Organization effectively overturned Roe v. Wade, undoing a half-century of nationwide access to abortion. Numerous legislative bodies across the country have passed or attempted to pass abortion bans, fetal personhood laws, or both. Such deliberations put uteruses—and the people in whose bodies they reside—firmly at the center of debate.
Given these political stakes, I’ve thought a lot about what it means to keep my uterus close—even now that it’s no longer housed in my body.
To answer the question of why I keep my uterus in my dresser, I need to return to 2004, the summer after the birth of my second daughter, when I decided to undergo a relatively new sterilization procedure.
The procedure involved transvaginal insertion of small, stint-like objects into each fallopian tube, designed to cause scarring and blockage, and thus to prevent contact between egg and sperm that might result in pregnancy. Though I favor vasectomy as a safer alternative to more intrusive forms of contraception and sterilization targeting people with uteruses, it was important to me that I not become pregnant again. I was 38 years old and certain I did not want more children.
Eventually, after four years, my uterus came back to me. Its arrival felt like a homecoming.
Prior to undergoing the procedure, I had already done extensive research on the topic. In the early 2000s, I started a comparative study of sterilization procedures globally, assessing both their potential for abuse as well as their usefulness in enabling people to manage their own reproduction. (According to the World Health Organization, over 65 percent of people globally use some form of contraception, including sterilization.) I interviewed company founders, scientists, ethicists, and critics; reviewed U.S. Food and Drug Administration (FDA) records; and assessed the clinical and scientific literature.
Still, I was a very early user in the U.S. of the sterilization procedure I chose—so early, in fact, that my physician in Washington State had not yet done five insertions, thereby necessitating that a company representative be in the room with us. This was not a requirement of the FDA but rather of the manufacturer itself. (Of course, I interviewed the representative while I was undergoing the procedure.)
Unfortunately, the procedure turned out to be too good to be true.
Read more from the SAPIENS archives: “Broadening Demands for Reproductive Justice.”
Many users of the technology developed serious problems ranging from ectopic pregnancies to abdominal pain to migration of the device. A Facebook group for users to share their stories reached more than 43,000 members. Soon, there were class-action lawsuits (these legal challenges are why I do not name the technology here). The best medical practices for managing the device shifted, too, with doctors recommending partial or full hysterectomies for removal. Though in my case, the device had done what it was supposed to do—prevent pregnancy—I grew worried about its long-term effects, especially when evidence emerged that the device could leach toxic metals into my body.
After consulting with my own doctor in Arizona, who was not the same physician who had inserted the device, I chose to undergo a partial hysterectomy. The surgery removed my uterus, fallopian tubes, and the device, but left my ovaries and cervix in place.
And this is when my womb began to have an adventure of its own.
After its removal, my uterus was transported from the hospital in Tucson, where I had undergone surgery, to an undisclosed location in Florida. I had hoped to see it before it was whisked away, but alas, I was unable to. In Florida, it was retained as evidence by a facility that houses biological specimens involved in litigation.
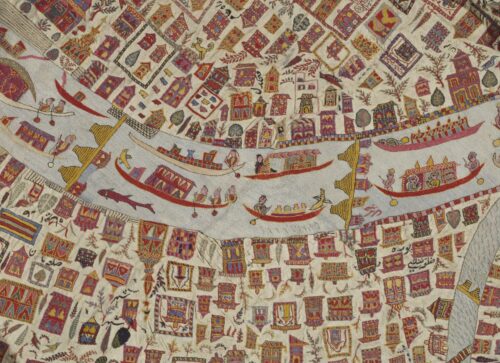
I thought often about my uterus, imagining it stacked on a shelf alongside other body parts in formaldehyde, like a cabinet of curiosities. I did not experience its absence as a phantom pain, as when people lose limbs. But I did develop a new and slightly unsettling relationship to my reproductive organs. I started to perceive a hollow in my abdomen. Sometimes, I still imagine my unmoored ovaries swaying gently in peritoneal fluid, like seaweed.
Eventually, after four years, my uterus came back to me. One day, I returned home from work and found a somewhat battered carton on the front porch; inside was my uterus. It was away from me for so long that I had forgotten I had checked the box on the hospital form that said I wanted it back.
But I am very glad that I did, because its arrival felt like a homecoming.
I promptly placed the plastic bucket containing my uterus into the refrigerator next to the arugula, before realizing it did not need to be kept cold. This is how it ended up in my dresser. It took me a while to look more closely at my uterus, in part because I first needed to purchase high-quality protective gear. (The pandemic had normalized consumer availability of such technologies; I bought mine on Amazon.)
On a sunny day in October 2023, I donned the respirator mask and safety goggles. This alarmed my dogs, who eyed me as if I was an intruder intent on stealing their biscuits. Warily, they followed me from the kitchen into the bedroom, where I removed the container from my dresser. It was about the size of a Kentucky Fried Chicken bucket and enveloped in hazard tape. I carried it gingerly into the bathroom, locking the door behind me to keep out the dogs.
Sitting on the bathroom floor with the ceiling fan whirring, I first photographed the entire apparatus. Then, I removed the hazard plastic. Next, I photographed the label on the container’s lid, which included the words “Pathology Specimen,” my first and last names, and a date, 12/12/19—the date of my hysterectomy.
Unscrewing the lid turned out to be difficult. After several tries, worrying that I would spill the contents, I managed to loosen the lid enough to pry it open. Peering inside, I saw a fist-sized, rust-colored object floating in greenish fluid. It reminded me of vats of chemical waste that comic-book humans fall into before becoming superheroes or archvillains. Another smaller, darker blob rested on the container’s floor, a few inches from the larger object. I was grateful for my protective gear, as the fluid looked noxious; I could almost smell it through the mask.
The larger object looked like meat. It reminded me of a turkey’s vital organs that my family and I fry up for the dogs at Thanksgiving. Floating in formaldehyde, the blob could have been a science experiment gone wrong. Or the detritus of a failed cooking show. Or an illegally trafficked human organ. Or an especially clever way to scare a child. What it did not look like was what it actually was: a human uterus.
Examining my uterus made me wonder how many people view their own internal body parts after having them removed. Would they even want to?
When I tell people that I store my uterus in the dresser, they react with fascination, horror, and/or amusement. A few ask how I was able to keep it, given that hospitals often retain extracted organs for legal and other reasons. I explain about the sterilization procedure and the hysterectomy, and then I tell them that I am working with a taxidermist to creatively preserve and display my uterus. I hope to take it to conferences with me as a part of presentations and talks. One day, my youngest daughter will have it; she has told me she wants it because it was her first home.
Most cultural representations of uteruses, including plushy dolls and cartoons with faces, sanitize the visceral fleshiness of the organ. Such representations also disconnect the uterus from the people in whose bodies they are located. But in or out of my body, my uterus belongs to me. It is both evidence and treasure, the embodiment of what I have gone through as a woman, a mother who had two cesarean sections, and a women’s health scholar.