What Makes Vaccines Social?

阅读本文:中文 (Chinese)
Now is a pressing time for vaccinating the U.S. population (and the world) against COVID-19. But there are social hurdles that need to be addressed.
As of this writing, more than 380,000 people have died from SARS-CoV-2 in the U.S. alone. Worldwide, more than 92 million people have been infected, and while many of these individuals have recovered completely, some are experiencing long-term health problems.
In combination with this, millions in the U.S. and around the world have lost their jobs due to the pandemic, leading to economic insecurity and food and housing crises. Psychological distress and domestic violence have also become more common. The world population at large is frustrated, concerned, scared, angry, exhausted, and very much wanting the current situation to end.
A potential resolution is on the horizon, but for COVID-19 vaccination to work, people need to be willing to take the vaccines. Like many social scientists working in the fields of vaccine uptake and disaster response and recovery, we anticipated that widespread acceptance of COVID-19 vaccines would be a critical issue—an issue upon which the success of the vaccination campaign, and the solution to the pandemic, would hinge. That is what we are now seeing today.
For our part as anthropologists, we have co-led two projects to help understand and address vaccine acceptance: a National Science Foundation–funded CONVERGE initiative that resulted in two national reports, and more recently CommuniVax, a national coalition to strengthen minority communities’ roles in an equitable vaccination rollout, sponsored by the Chan Zuckerberg Initiative. Others are also working on these issues, including groups from the National Institutes of Health, the Institute for Vaccine Safety at Johns Hopkins University, and the Vaccine Confidence Project at the London School of Hygiene and Tropical Medicine.
But even more is needed. The social science behind vaccine uptake—who is or isn’t willing to be vaccinated and why—needs to be funded and put into action.
By stimulating an immune response, vaccines can directly protect those who receive them. When widely accepted, vaccines can also confer indirect protection to entire populations by limiting the spread of pathogens. This protection—referred to as herd or community immunity—is what ultimately makes vaccination successful. It is what made the eradication of smallpox a reality and the low rate of measles in many areas of the world possible. It is also the way for the world to return to something that looks and feels more “normal” now.
Vaccination as a solution to COVID-19 was well-appreciated at the earliest moments of the pandemic. Almost immediately, scientists at leading pharmaceutical companies began developing COVID-19 vaccines. Governments and private organizations sought to assist in these efforts. On May 15, for example, the U.S. government announced Operation Warp Speed, a US$10 billion public-private partnership to “accelerate the development, manufacturing, and distribution of COVID-19 vaccines.”
All these efforts have resulted in great success. At the time of writing, two vaccines—from Pfizer-BioNTech and Moderna—have been approved for use in the U.S., seven others are approved or being used in limited capacities around the world, and 83 more are under development. While a technological coup—typically new vaccines take 10–15 years to develop—a critical assumption has been made: that people will simply accept COVID-19 vaccines once they became available.
Humans are not as simple as viruses. They have personal histories, opinions, wants, and needs. They are embedded within social networks that have their own unique configurations of worldviews, and they are members of cultures that offer particular interpretations of the body, disease, and treatment—which do not always conform to the perspectives or interests of biomedicine and public health.
Polling over the past nine months has suggested that not everyone will be willing to accept COVID-19 vaccines. While specific numbers have changed over time, some trends remain clear: In the U.S., Black adults, younger adults (aged 30–49), rural residents, and Republicans consistently indicate that they are less willing to accept COVID-19 vaccines compared to their counterparts—though not always for the same reasons.
Among those who have been allocated doses of the Pfizer and Moderna vaccines, refusal has already occurred. In Ohio, for instance, nearly 60 percent of nursing home staff have reportedly elected to not be vaccinated.
In an ideal world, the social issues that impact vaccine uptake would have been noted and addressed at the very beginning of vaccination planning efforts. Integration of social science into the earliest iterations of Operation Warp Speed, for instance, could have accelerated interventions within racial and ethnic minority communities, university student bodies, and other potentially reluctant groups.
And it most certainly would have prevented the use of the term “warp speed” in a public health effort: Speedy development is not a characteristic that most people care to have associated with medical interventions. In 2009, for example, even though the H1N1 vaccine was simply the yearly flu vaccine with a new strain of flu included, rumors quickly spread that the vaccine had been “rushed” and consequently was unsafe.
We do not live in an ideal world, however. Instead of an integrated approach, social scientists and others working to preemptively address COVID-19 vaccine uptake have largely been working from the margins, trying to affect change and influence policy without directly having a seat at the table.
Humans are not as simple as viruses. They have personal histories, opinions, wants, and needs.
This is problematic. While some of the issues related to vaccine uptake (for example, the need for tailored messages, advocacy from trusted spokespersons, and transparency around vaccine technologies) are well-understood and widely appreciated, other issues are more subtle and require greater context—context that only social science can provide.
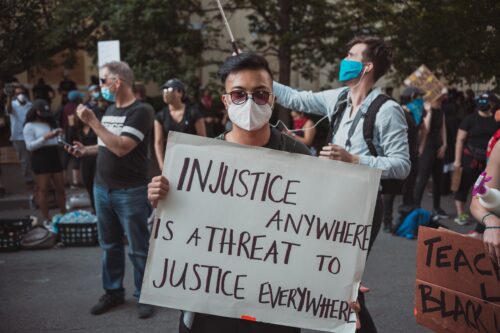
One of these—and the primary impetus for the development of CommuniVax—is the seeming contradiction of racial and ethnic minorities being hesitant to accept COVID-19 vaccines when they have been disproportionately affected by the pandemic (including greater infection rates, higher death rates, higher rates of job loss, and more).
The context for this situation involves a combination of factors such as structural racism, racially biased health care, historical incidents like the 1932–1972 Tuskegee Syphilis Study (in which 399 Black men in the South were denied treatment for over 25 years), and a lack of funding for public health generally. The latter has limited public health practitioners’ abilities to address health needs identified by minority communities, such as diabetes and cancer. The result is that, long before SARS-CoV-2 appeared, many minority communities across the U.S. were wary of public health initiatives. In this light, it makes sense that members of these communities would be wary of COVID-19 vaccination as well.
Complicated issues like this are not easily addressed. Education and better communication are not solutions by themselves; people’s opinions are not easily swayed by facts alone but instead are influenced by deeply held, culturally based beliefs. There is no proverbial silver bullet.
As applied anthropologists, we recognize the importance of balancing the “messiness” of situations with the need to provide practical recommendations. In our reports and official advice, we have suggested the following in relation to the specific issue of wariness among racial and ethnic minority populations: making COVID-19 vaccines available at no cost to everyone living in the U.S. who wants one; engaging minority communities to understand their specific realities and concerns, and from this, developing objective allocation and distribution strategies that they see as fair and ethical; and facilitating public ownership over the COVID-19 vaccination program.
The last point is the most difficult—but the most important. It involves allowing community members to have input on the practicalities of the vaccine rollout, including the places (pharmacies, churches, et cetera) vaccines will be provided at; promoting community-developed messaging and messengers; and developing true partnerships between local public health officials and community members that can last beyond the current crisis to address the long-standing needs in these communities in the future.
Over the past nine months, the two of us and our colleagues have been working toward implementing these and the other suggestions we posed. We have written national reports, given interviews to major news organizations, talked to members of government at state and national levels, and presented in webinars hosted by professional organizations. Through our guidance of CommuniVax, local teams of anthropologists and others are working directly with minority populations in communities across the U.S. And we are continuing to advocate for the policy changes and funding that are necessary to address the social aspects of COVID-19 vaccine uptake more broadly.
Our hope is that the vaccination program will be successful, that the pandemic will be controlled, that life will return to something more normal, and that, moving forward, public health and biomedicine can work better than they have in the past, especially for those who are most in need of them doing so. With input from social scientists, and the integration of this input into policies and practice, we think this hope can be realized.