Why Eradicating Polio Is More Complicated Than It Seems

In a rapidly urbanizing sector of Karachi, Pakistan, dry and dusty hills rise up from the city below. Migrants to the area, many of them escaping violence and drone attacks along the border between Pakistan and Afghanistan, have built homes in rows on the steep hillsides. In one of these, Nasreen, a young mother, sits in the living room of her small, immaculate flat. [1] [1] To protect people’s identities, all names in this piece (other than the author’s) are pseudonyms.
Karachi is one of the world’s last reservoirs of polio. Earlier in the week, a team of vaccination workers had visited Nasreen’s house with an oral polio vaccine; they planned to return in a few days. But Nasreen is unsure whether to allow the workers to immunize her 1-year-old son. “I know polio is a horrible disease,” she says, “but those vaccinators weren’t clean—they looked like beggars. What do they know about polio and health?”
Nasreen has a college degree and doesn’t doubt the science behind immunization. “I’m in favor of vaccination,” she says. However, she adds, “I don’t think these door-to-door polio campaigns are a good thing.” She pauses. “Some people say these polio campaigns are part of an international plot to sterilize our children. Tell me, are these polio drops really safe, or not?”
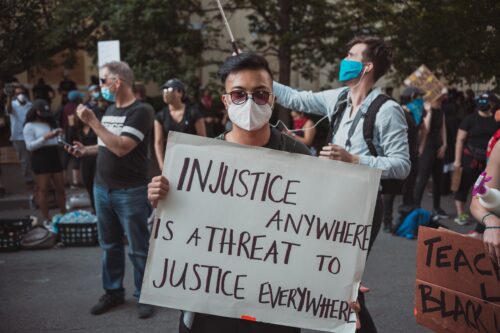
Rumors that the polio vaccine causes sterility in children circulate not just in Pakistan but also in many parts of Africa. To outsiders, these rumors might appear to be the result of ignorance or of odd cultural beliefs. But on closer examination, such rumors are found to be a natural and logical consequence of distrust. When international agencies and governments that locals already have reasons to doubt swoop in and focus intensely on one disease, it does not inspire confidence—it does the opposite.
There is a way to both strengthen the fight against polio and begin to build a core of trust between the people at risk and those trying to help. It isn’t simple, nor is it easy to raise funding for the changes that are required: prioritizing basic health care, providing reliable sanitation, and improving infrastructure. But these basic services would build trust, and, along with immunization, they could help break the chain of polio transmission in the disease’s last strongholds.
Polio is caused by a virus that travels through fecal-oral transmission. It spreads when sanitation systems are ineffective, through flies that land on food, and in drinking water contaminated with fecal matter, among other pathways. (In the United States in the 1950s, the poliovirus was commonly transmitted in swimming pools.) In most cases, a person with the infection is asymptomatic, or they experience mild flu-like symptoms that pass without major incident. But in less than 1 percent of cases, the poliovirus has much more severe effects. In these cases, victims experience sudden paralysis, usually on one side of their bodies; a limb that was healthy hours before will become terrifyingly floppy and unresponsive. Many of these people never walk again. If paralysis strikes the lungs, polio can be deadly.
Such paralysis is often irreversible. But it is preventable with a vaccine. The Global Polio Eradication Initiative, started in 1988, has reduced the number of cases of paralysis globally from an estimated 350,000 in the late 1980s to about 120 cases a year today. Yet polio subsists in Pakistan, Afghanistan, and Nigeria. Getting rid of the last cases is the hardest: It means succeeding in eliminating the poliovirus in populations where it has persisted despite repeated vaccination campaigns for 30 years. For 2018, the initiative has budgeted about US$231 million and deployed more than 200,000 people to chase down polio in Pakistan alone.
Over decades, armed conflict in Pakistan has had a long-term, serious impact on health services. The country has poured its resources into national defense, at the expense of sectors like education and health care. In 2015, the government spent just 3.7 percent of its total budget on health—one of the lowest allotments of any country in the world. The result is that Pakistan’s public health care system often does not provide basic services like childhood vaccines to all citizens, which is a serious problem for the poor and marginalized, who can’t afford to pay for care in the private sector.
In Karachi, there has been a week-long door-to-door polio campaign, carried out by the Pakistani government but funded and supported by the Global Polio Eradication Initiative, nearly every month for the past 10 years. Houses are visited by vaccinators attempting to find and immunize every child under 5 as often as 10 times a year.
Multiple doses of the vaccine are often necessary because the oral polio vaccine has low efficacy in places where many children have competing infections in their guts. As a result, many of them have been vaccinated against polio up to 30 or 40 times. Yet polio transmission continues because some children are under-vaccinated—either because they are repeatedly missed by the campaign teams or because their parents refuse the vaccine. (According to one estimate, approximately one-third of unvaccinated children in Karachi are a result of refusals—some 34,000 children.)
In 2012, my colleagues and I visited eight sites in seven countries, interviewing more than 300 people, from parents to vaccination teams to policymakers, to uncover the reasons behind polio vaccine refusals. A member of our Pakistani research team met Nasreen in Karachi during this project. [2] [2] The author would like to acknowledge Sarwat Jehan and Patricia Omidian for their interview data and field notes, some of which were used in this article.
The area where Nasreen lives has few government services. There is no municipal water, and the narrow street outside her house is littered with garbage and animal dung. You have to watch where you step. Open ditches next to the narrow alleyways flow with raw sewage; in the 100-degree heat of the summer, the air takes on a thick tang from the smell, and people cover their faces with headscarves or handkerchiefs.
The public health center servicing this area is in an older neighborhood with narrow, maze-like alleyways. The center is literally falling apart: Large chunks of plaster are missing from the ceiling and the walls, and there’s a ramshackle pile of broken furniture in a corner of the dingy waiting room. There’s no backup electricity for handling the city’s frequent blackouts—the two generators are both broken, and in any case, neither has fuel.
On the day that one of our team members visits this health center, a young mother, Roshina, is in the waiting room, sitting patiently with a small, listless 4-year-old in her arms. Roshina’s burqa marks her as a migrant, like most women in this part of town. Her young daughter has severe diarrhea, and she’s been vomiting; Roshina is concerned. She should be: Dehydration from diarrhea is one of the leading causes of death in Pakistani children. Patients fill the waiting room, and although the doctor was supposed to be there at 9 a.m., it is now almost 10 a.m., and she hasn’t arrived yet.
When the doctor finally appears, she powers through seeing her patients, spending less than a minute with each one. There is not so much as a curtain for privacy; people describe their health issues in front of everyone waiting. In many cases, the doctor tells patients to come back to her private evening clinic (when she charges for services). The doctor has no supplies—no stethoscope, not even a prescription pad. When Roshina’s turn comes, the doctor barely glances at her daughter before throwing a prescription at them, written on the back of a polio pamphlet (the only paper in the health post). Roshina tries to ask a question, but the doctor does not speak Pashto, the language that most migrants like Roshina speak.
The city of Karachi has world-class health services for those who can afford to pay, but these are out of reach for mothers like Roshina and Nasreen. In her living room, Nasreen reflects on negative experiences she has had with the government health post. “There are never any medicines there,” she says. “The health workers, they take the medicine and sell it on the side.” She is visibly anxious when she talks about the delivery services provided at the maternity center. “Some people have problems during pregnancy,” Nasreen says, “but that hospital doesn’t even have an operating theater.”
It’s reasonable that mothers would distrust health interventions that are heavily pushed on them by the same government that doesn’t seem to care when their children are seriously ill. That’s exactly what our study confirmed: Refusals were most common and vehement when a lot of emphasis was placed on polio in a context where other health services were neglected. In such circumstances, many parents begin to fear that a vaccination campaign may not be what it seems.
The people who fight polio in Pakistan’s cities, most of them Pakistani, are true heroes, working under often dangerous conditions to rid the world of a scourge. Polio workers have been attractive targets for insurgents because polio eradication is an obvious priority of international actors and the Pakistani government. The violence has lessened now, but between 2012 and 2015, militants murdered at least 30 and perhaps as many as 80 polio workers, many of them in Karachi.
Given these challenges, eradication of polio is extremely tough. The original target date for eradication by 2000 has been extended again and again—to 2005, 2008, 2010, and so on until the current target of 2021. The success of polio eradication in other parts of the world, such as India, suggests that the work in Pakistan would have been finished by now if basic water, sanitation, and appropriate infrastructure existed. Preventing fecal matter from entering the streets, for example, would make eliminating polio from this area much easier. But funding for such services, either from international donors or from the government, can be hard to come by.
Recently, polio eradicators in Karachi have instituted mobile clinics in an attempt to alleviate some of the most severe health care shortages. They have renewed focus on routine immunization against a range of diseases. And, in some of Karachi’s slums, they have installed water filtration plants that dispense clean drinking water to everyone. They realize that public trust is affected by the quality of a variety of services. These efforts represent a small fraction of the funding and energy directed toward eradicating polio. Still, for Nasreen, who said what she wanted most was a mobile clinic with free medicine to come to her area, such services could make a real difference. They would build trust in the health system by providing the services she needs.
But these are small steps. It’s time for international donor agencies—and those of us who give to those agencies—to prioritize basic health care, sanitation, and infrastructure alongside disease-specific programs. These services are not sexy, and building them is a complex and difficult task. But if we are going to eradicate communicable diseases, we have to start with the basics.