Beyond the Vaccination Rift

“Man is by nature a social animal … for [whom] the whole must necessarily come before the part.”
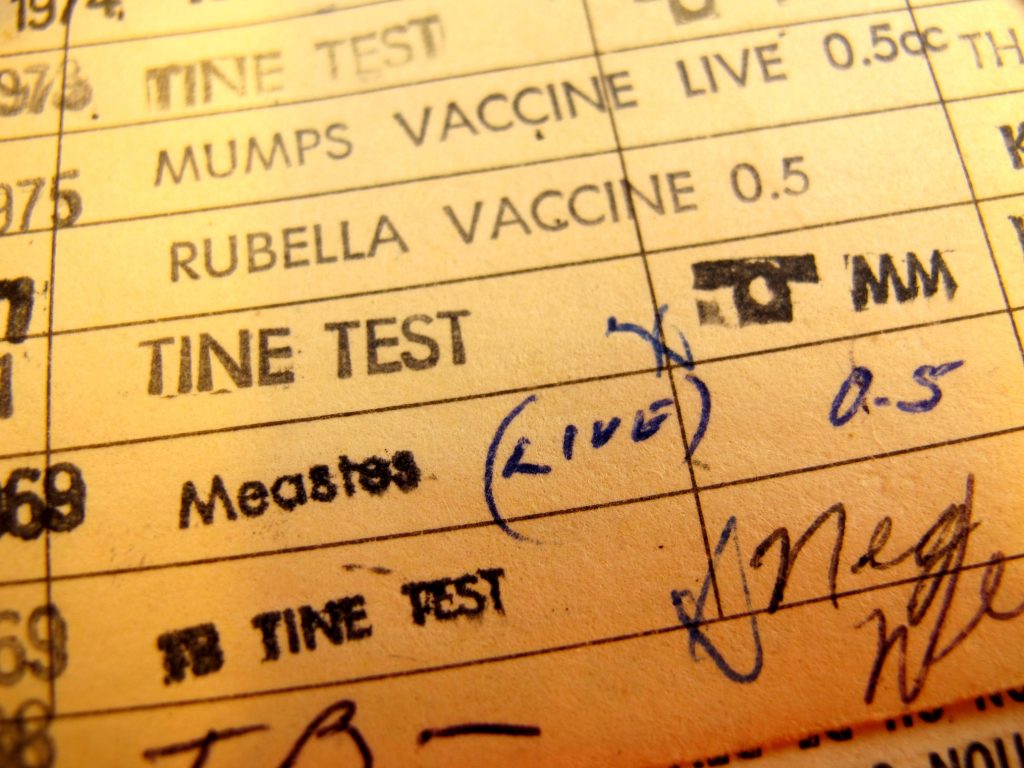
Parents who do not vaccinate their children have faced a firestorm of vitriol in recent years. Media coverage of outbreaks of vaccine-preventable diseases such as measles and whooping cough has too often ended in a blame game, deepening divides between communities of parents who vaccinate routinely and those who do not.
Such us-versus-them thinking both ignores the many parents in the middle and misses the critical point that most parents share the same aim: to keep their children healthy. And although myriad factors play a role in U.S. parents’ vaccine choices, a growing body of research suggests that vaccination decisions are—at the core—strongly influenced by the fundamental human social desire to belong.
I stumbled onto my own evidence for this accidentally. In the spring of 2012, I conducted a children’s health project at a private Waldorf school in California where 280 prekindergarten through 12th-grade students were enrolled. Waldorf education is rich in the arts and heavy on experiential learning, and it has no use for standardized testing. Although by definition an independent system, with 120 private U.S.-based schools, Waldorf education has inspired a number of recent public-education innovations. A growing number of U.S. public (often charter) schools offer Waldorf-inspired program components.
In my study, I was primarily interested in the link between teaching strategies and child health, which the Waldorf teaching philosophy promotes. Although my main focus was on what happened during school hours, I also wanted to understand how teacher recommendations regarding media avoidance, early bedtimes, and wholesome eating, for instance, were being followed at home.
Waldorf schools are anecdotally regarded as accommodating to vaccine “nonconforming” parents (those who choose not to vaccinate, who vaccinate selectively, or who follow a delayed vaccine schedule). Of course, vaccination is a fraught topic, so to avoid digressing into this hot-button issue, I initially did not ask about vaccination in the study. However, participating parents kept bringing it up. They wanted to talk about it. In response, halfway through the study I added a question directly related to child vaccine status. Quantitative findings from this question were meant to complement the qualitative data, or personal stories, that parents spontaneously provided.
The school hosting the study had a personal belief exemption or PBE (a vaccine waiver that allows parents to opt out) rate of 51 percent for kindergarteners. The state average in California is 2.8 percent.
The obvious explanation for this huge difference was that Waldorf education’s rumored support for nonvaccination was drawing a disproportionately large number of vaccine-nonconforming parents. However, the school’s advertising does not mention vaccination, and vaccination never came up in parents’ enrollment stories that I recorded for my research. Instead, parents reported being drawn to the school’s renowned alternative educational approach. In fact, many did not know about the vaccination-related stereotype prior to joining. In other words, my data did not support the assumption that parents sought out the school for its stance on vaccination.
Rather, my study found that enrolling one’s children, and assimilating, as a family, into this vibrant community, often intensified prior choices to delay or avoid vaccination. Joining the school even propagated vaccine nonconformity among some parents who previously had complied with state recommendations.
As a focus-group member explained, “A lot of people that come … to Waldorf have vaccinated their children … and then they chose to discontinue.” For instance, one mother had a 10-year-old child who was fully vaccinated prior to enrolling in the school’s early childhood program. Her second child, born after the family’s enrollment and subsequent immersion in the school’s community, was unvaccinated at the time of the study. Another parent was apologetic about vaccinating her older child prior to joining. “I didn’t know any better,” she said. This was a common refrain.
Family data showed further that younger siblings at the school received notably fewer vaccines than older ones. By the time children entered seventh grade, which for many might represent 10 years of membership in the school’s community, the PBE rate was 71.5 percent. The social fabric of the school served to foster this extraordinarily high percentage.
Yet, a notable subset of students were fully vaccinated. Even most of those with waivers had received at least some vaccinations: only two of 17 participants from whom vaccine status data were collected had none. But vaccinating parents said that the school’s culture supported skepticism regarding governmental and healthcare industry (“big pharma”) interests, favoring countercultural approaches to children’s health. In doing so, it stigmatized the conventional perspective on vaccination.
“There’s prejudice against mainstream medicine,” said one parent bluntly. Some parents who vaccinated reported that fear of reproach from their peers led many to keep silent about having done so. Another tactic was to publicly disavow optional vaccines, such as for the flu. These behaviors create the false impression that nearly everyone in the school community disfavors pediatric vaccination. As a result, post-enrollment, the stereotype regarding the school community’s vaccination practices becomes self-reinforcing.
The school-based study, which highlighted social factors that can reinforce vaccine nonconformity in particular group settings, led me to design a broader, community-based study that specifically questioned vaccine confidence and nonconformity against the backdrop of mainstream culture. A prominent theme in the school study—that, as one parent said, “It takes a lot of work to go against the grain of society”—had special relevance in this broader project: many participants in the community sample were content to accept “the package” of recommended vaccinations.
In the community sample, participant testimony suggested that easy acceptance of vaccination was based on two main factors: an everyone-does-it-here point of view and prior personal experience of vaccination. Referring to her husband as well as herself, one woman reported, “We were both vaccinated as children, so it seems like a cultural norm.” Another parent said with a shrug, “It seemed pretty routine, pretty normal.”
Parents did not choose to vaccinate because of better education. Full vaccinators in the community sample were in fact less information literate than selective vaccinators. Their average score on the Kent State University Libraries information literacy survey, which assesses people’s ability to evaluate sources and information, was 71 percent, compared to 76 percent for selective vaccinators. In addition, most full vaccinators knew surprisingly little about how vaccines work and even less about herd immunity.
They generally had their children vaccinated as part of their parenting routine, simply put. As one mother explained, “It’s part of the program. I’ve never had a second thought about not doing it. But I think the decision—I know I’m doing the right thing—is based mostly on previous experience with my parents, [what they] did for me.” For such parents, to not follow this example or to reject “the program” would entail too much social risk.
Routinely vaccinating had become a cultural tradition for these parents, much as vaccine nonconformity had for many parents at the study school. They chose to vaccinate as what anthropologists often call an “act of affiliation.” By vaccinating their children, parents asserted their commitment to community customs. This ensured continued good relations with family and friends.
Vaccine-nonconforming parents do the exact same thing—only they align with a different community. For them, to refuse one set of norms—those favoring vaccination—is to endorse another—norms supporting vaccine nonconformity.
My findings provide concrete evidence supporting the theory (referenced not only in work on vaccination but also climate change and other divisive topics) that parents conform their thinking about risk, particularly when that risk has taken on social meaning, to community norms. Parents do this to demonstrate solidarity and confirm their sense of social identity with the community.
My findings also reinforce those from a 2013 study that found the proportion of individuals in parents’ “people networks” who promoted vaccine nonconformity was the most significant predictor of parents’ own vaccine nonconformity—even when compared to their own beliefs regarding vaccination. Put another way, parents make vaccination choices that reinforce their social ties.
In the end, then, vaccine-nonconforming parents and routine vaccinators have much in common. To see them as fundamentally opposed to one another is unhelpful at best. To overlook the influence of social relationships in vaccine choices is to miss a critical opportunity for finding common ground. A polarizing focus also diverts attention from the fact that science is not the primary consideration in most parents’ immediate experience of vaccine decision-making.
These findings are important not just for public health planning but also for how we understand ourselves. At the end of the day, our social nature strongly affects our vaccination choices. We vaccinate—whether fully, selectively, or not at all—to create, reflect, and maintain our connections to the social wholes we are a part of, and to nurture a sense of belonging. Those who hope to influence vaccination behavior would do well to consider our social side—but in a way that builds bridges, not fences.