No, “Racial Genetics” Aren’t Affecting COVID-19 Deaths

Around the world, there are reports that COVID-19 is affecting some people more than others, and not just the elderly. In the U.K., where I live, people of black, Asian, and minority ethnic (BAME, as these groups are commonly called in the U.K.) backgrounds constitute 33 percent of the critically ill patients with COVID-19, but only 22 percent of the local populations where those patients are being treated.
Similar statistics hold true in spots other than the U.K. In New York City, Hispanics make up 29 percent of the city’s population but 34 percent of the fatalities; black people make up 22 percent of the population but 28 percent of the deaths.
Why is this?
Some news articles have implied that “race” might have some biological effect on susceptibility to COVID-19. One example of this comes from the Naked Scientists, a group of scientists, doctors, and communicators based at Cambridge University’s Institute of Continuing Education who host an extremely popular podcast. On April 11, the group tweeted that, regarding this BAME disparity, “what’s unclear is whether it’s a race thing (and hence some underlying genetics, susceptibility to certain diseases), or if it’s a socioeconomic thing, or both.”
There is a common and pervasive misunderstanding about what “race” actually is.
As a bioarchaeologist—and as a person—I find such statements problematic and shocking.
This kind of comment, and others from the same account, is disturbing—especially when coming from an organization aimed at expanding understanding of the sciences. It showcases, yet again, a common and pervasive misunderstanding about what “race” actually is. There is no genetic basis for determination of or separation by race; it is purely a social construct.
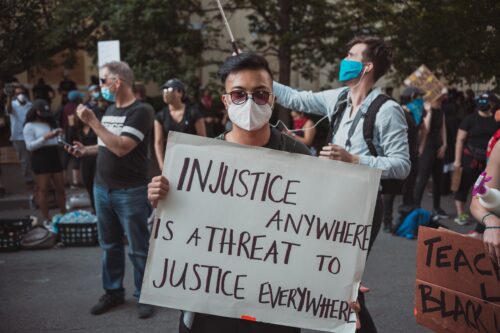
The problem is that ascribing the disparity of COVID-19 impacts on BAME groups as genetic masks the more likely, and more pernicious, causes: systemic inequalities. These are the same systemic inequalities that have prompted outrage and protests over killings of African Americans, including George Floyd, a black man living in Minneapolis who was killed by police on May 25.
Broadly speaking, BAME groups have different experiences of wealth, health care, diet, housing, employment, multigenerational households, and epigenetics compared to majority groups in the U.S. and the U.K. Statistically, they have different experiences with the police, with authorities, and with social services. This is what really deserves to be highlighted and needs to be addressed.
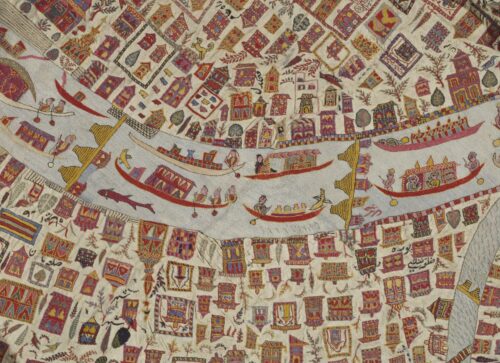
“Race” exists as a social construction: It’s a mechanism by which people are lumped into groups based on superficial physical qualities such as skin color and hair characteristics. It has long been known that there is vastly greater genetic diversity within such groups than between them, making the so-called groups genetically meaningless.
There aren’t even hard and fast rules about which “races” people recognize: The categories have changed over time and vary in one part of the world versus another. The most common divisions in Europe and North America today are black, white, Hispanic/Latinx, Indigenous, and Asian. But, in North America for example, Asian is often considered to refer to East Asia, whereas in the U.K., the term is typically associated with South Asia.
I have “white” skin, but my grandparents were born in present-day Pakistan, eastern Siberia, and what is now Poland but was then Germany. What does that make me? On occasion, my sister and I have been known to agree in advance to tick separate boxes about our ethnicity on everything from surveys to job applications.
Despite these facts, misunderstandings about race are rife not just among the public but also in the medical field. The National Institute for Health and Care Excellence states that “Afro-Caribbean patients may respond less well to angiotensin-converting enzyme (ACE) inhibitors,” for example. And yet the evidence for a biological explanation of any apparent racial difference in drug response is slim or nonexistent.
One relatively early study that has been cited more than 150 times as evidence for this fact looked at just 20 individuals divided into three racial groups. Just 13 of them were assigned as black/Afro-Caribbean—an extremely small sample. These people weren’t all given the same ACE medication (4 different ones were used), and the fact that they were of different sexes and ages was basically ignored. This is simply bad science hung onto a racial hanger.
There have been plenty of further, bigger studies on racial differences in response to ACE inhibitors since then. Many, like one published in 2015 in the Journal of the American College of Cardiology, do not implicitly exclude the possibility that the differences may have a social cause at their root, but they still leave the reader with the impression that the reasons are biological.
Sadly, such medical research has been accepted by many, including the Naked Scientists—who proposed that these different responses to ACE inhibitors might explain the range of outcomes of COVID-19. (They note that the virus and these drugs both bind to some of the same cell receptors.)
Yes, people do respond differently to diseases and to drugs, in part because of their genes. Efforts to look for links between specific genes and specific medical outcomes are perfectly valid. But using “race” as a proxy for those genetic differences is not.
This has been written many times in the past, but, infuriatingly, the message still does not seem to be understood by many medical researchers. Dozens of medical preprint articles refer to “race” in relation to COVID-19, such as this one: “Racial/ethnic disparities in COVID-19 illness severity may relate to yet unidentified host-viral susceptibility factors.”
The clear and insidious implication is that racial groups are meaningful in a biological way. Some discrete ethnic groups, such as Ashkenazi Jews, may have some meaningful genetic markers deriving from common ancestry, but this rarely holds true for other ethnic groupings.
During the current pandemic, some news articles have usefully and rightly discredited ideas based on “racial genetics,” including the BBC’s “Coronavirus: Why Has the Virus Hit African Americans So Hard?,” Reuters’ “fact check” article “False Claim: African Skin Resists the Coronavirus,” and NBC News’ “Coronavirus Outbreak Revives Dangerous Race Myths and Pseudoscience.”
But others continue to make arguments about race and genetics, often leaning on statistics coming from the U.K.’s medical community. The first doctors in the U.K. to die of COVID-19 were all from BAME communities. As of April 18, almost three-quarters of the medical professionals and health care workers who have died of COVID-19 in the U.K. came from BAME backgrounds. Since doctors are perceived to be similarly well-educated and relatively affluent, people have suggested in popular debates and forums that this shows that genetics, not socioeconomic factors, lie behind the disparity.
There are plenty of possible socioeconomic explanations for the BAME disparity in COVID-19 severity and deaths.
This argument has several failings. For example, it is possible that the doctors from BAME populations live in areas with high poverty and/or social overcrowding. More importantly, all of the first doctors to die were also immigrants: They may have experienced early life in very different conditions than those they live in within the U.K. And their mothers’ lives may have been quite different too. The maternal condition is an important factor in how human genes are expressed later in life (a factor called “epigenetics,” not to be confused with genetics). The health of a person’s mother can have impacts on them that last a lifetime.
There are plenty of possible socioeconomic explanations for the BAME disparity in COVID-19 severity and deaths. BAME communities in the U.K. are diverse. But there is a gap between median hourly pay between white and BAME groups in Great Britain (about 4 percent nationally in 2018 and nearly 22 percent in London). Where people work also matters. In the U.K., BAME communities are disproportionately represented in certain job classes, such as child care, elder care, food service, and transport. Many of these posts are deemed “essential work,” and so people continue to be at high risk for contracting the novel coronavirus.
It has been noted that BAME communities have higher rates of hypertension and diabetes, which may make individuals more susceptible to complications if infected with COVID-19—again, systemic inequalities probably lie behind that disparity in disease.
The terms BAME, ethnicity, and race are widely used in the media, usually without explicit or clear definition. Many journalists rely on common or garden variety understandings of race—but doing so often perpetuates the idea that there is some genetic or biological underpinning to the term. There isn’t. Communicators need to be clearer about this.
In the medical community, choosing and subdividing groups for medical research needs to be done based on clear and meaningful definitions. New studies, such as one by Genomics England, have begun to look at whole genome sequences of people who experienced severe COVID-19 symptoms versus those who only had mild symptoms. Such research actually looks at individuals and their individual genes rather than using the sweeping race or ethnicity groupings to attempt to create biological categories.
Without these types of changes from past practices, there will continue to be racism in medicine—as the British Medical Journal itself noted in its special issue on the topic. At this stage, it is imperative that medical treatment advice be reviewed. Many current guidelines about who should be offered which medicines are problematic because self-assigned “race” has been misused as a proxy for genetic variation in the research that supports the guidelines.
BAME communities do seem to be particularly adversely affected by COVID-19, but there is no logic behind the argument that there is a genetic cause for this. Race is not biological. But it is very real as a social construct. The social disparities faced by BAME communities—in health care, living conditions, wealth, and education, among other areas—are likely to lie behind their disproportionate suffering, and that’s what should be fixed. Social environment is key and must not be forgotten.