Schizophrenia’s Tangled Roots

Jacqui Dillon has been hearing voices since she was a little girl growing up in the London, England, borough of Hackney. They first came to her when she was about 5 years old. Some were soothing and comforting, but others were threatening and tormenting. For many years she told no one about them. But then, soon after the birth of her first child at age 25, the frightening voices greatly intensified. “I was having a lot of night terrors,” she says. “I felt paranoid and unsafe. I felt I was being monitored, that people were watching me outside my house.”
In desperation, Dillon contacted her doctor. That same day she was admitted to a London psychiatric hospital. There, for the first time, she confided to a psychiatrist that she had been sexually abused as a child. But, Dillon says, the psychiatrist told her that the abuse didn’t really happen. What to her were vivid memories, the doctor said, were just part of her illness. “The very real events I was talking about were defined as being hallucinations and delusions,” Dillon recalls. “They said they thought I had schizophrenia.”
Dillon says she devised a strategy to get out of the hospital. “I told them maybe they were right,” she says, that these things didn’t really happen. “I began to take back the things I said and agree with their definition of reality. I said, ‘Thank you very much, I feel much better now.’” After about two weeks, she was released.
Fortunately, Dillon says, she was able to find local psychotherapists who could give her the kind of help she thought she needed. “Rather than just dismissing my voices, they encouraged me to explore their meaning.”
Today, at age 51, Dillon is the chair of the Hearing Voices Network in England, helping others cope with symptoms that psychiatrists often consider signs of a psychotic disorder. For her and many other like-minded advocates, terms like “schizophrenia” are broad labels that do not get at the underlying problems sufferers are facing—especially if they are simply given drugs to dampen the symptoms and offered little or no help with making sense of them. “I’ve spoken to hundreds of voice hearers who have had similar experiences [with psychiatrists],” she says. “We are not listening to their voices and what happened to them.” Dillon criticizes the psychiatric profession—and society at large—for dismissing voices and hallucinations as mere symptoms of a biological or genetic disorder rather than a psychological attempt to “describe really terrifying things in metaphorical or symbolic ways.”
The Hearing Voices Network in England is one of more than 20 Hearing Voices Networks around the world. These peer groups organized by voice hearers and their supporters—along with a growing number of experts—insist on recognizing what many with schizophrenia already know: that the individual person’s experiences must be taken seriously for any attempts at treatment and recovery to be effective.
This does not mean that schizophrenia is something that can be easily dismissed or that patients can simply walk away from the condition by adopting the right attitude toward it. Schizophrenia is a serious mental illness that afflicts about 1 percent of people worldwide, often leading to early death and great social and economic burdens. And many, although not all, patient advocates accept that antipsychotic drugs—especially in moderate rather than heavy doses—can play a helpful role in the early stages of the disorder, getting the most florid symptoms under control so that psychological approaches have a better chance of working.
Yet, for decades, many experts have viewed schizophrenia strictly as a genetic disorder and an often incurable brain disease. And recent media coverage suggests that researchers are uncovering schizophrenia-related genes that could finally help them understand the roots of the disorder. Funding agencies in the United States, Europe, and elsewhere are spending millions of dollars on such research, and indeed many genes have been identified that do appear to increase schizophrenia risk.
Yet the extra risk associated with most of these genes is very small, which has led some researchers to argue that other factors, including environmental and family stressors, may be playing a role equal to or greater than genetic susceptibility. These researchers include psychologists, epidemiologists, anthropologists, and others who are trying to understand the complex mix of personal circumstances that can lead some people into the vortex of mental illness.
The emerging view is that the more overt psychotic symptoms of schizophrenia, including hearing voices or experiencing haunting delusions and hallucinations like those that used to oppress Dillon, often reflect underlying issues and conflicts in the lives of the sufferers. Most mental health experts today reject classical Freudian explanations for mental illness, such as repressed sexuality or a domineering mother or father. Yet modern psychologists who work directly with patients who suffer from schizophrenia and other forms of psychosis are sometimes able to identify environmental factors—ranging from childhood abuse or adversity to stressful events in adolescence or early adulthood—that can trigger a psychotic breakdown.
This is not to say that the psychiatric profession is simply ignoring the personal experiences of individual patients. Yet in many clinics and hospitals, the role of the psychiatrist is increasingly that of a prescriber of antipsychotic drugs rather than someone who sits and talks with patients about what is happening to them. That essential role, if and when there is funding for it, is usually relegated to psychologists and social workers.
“Psychiatric science has learned—epidemiologically, empirically, quantitatively—that our social world makes a difference” in raising the risk of madness, says Tanya Marie Luhrmann, an anthropologist at Stanford University who has studied the psychiatric profession for nearly two decades. But she adds that “standard psychiatric science cannot tell us what it is about culture that has that impact.”
Indeed, even the most biologically oriented mental health experts acknowledge that genetic and environmental factors are somehow interacting to increase schizophrenia risk. This view of the disorder is often called the “stress-vulnerability model.” Most cases of schizophrenia arise and are first diagnosed in late adolescence or early adulthood, when sufferers are going through dramatic and often stressful changes in their lives, such as leaving home for the first time. Yet researchers are still debating whether vulnerability to schizophrenia is predominantly determined by genetic or environmental factors.
Possible clues to the relative roles of genes and environment can be found in the genetic findings themselves. There are some rare genetic abnormalities that significantly raise schizophrenia risk. For example, human cells have 23 pairs of chromosomes, which carry the DNA that makes up our genomes. If a certain segment of human chromosome number 22 is deleted due to a genetic mutation (known as 22q11.2 deletion syndrome), an estimated 23 percent to 31 percent of people with that deletion will end up being diagnosed with schizophrenia. And yet the syndrome only accounts for about 1 percent of schizophrenia cases overall.
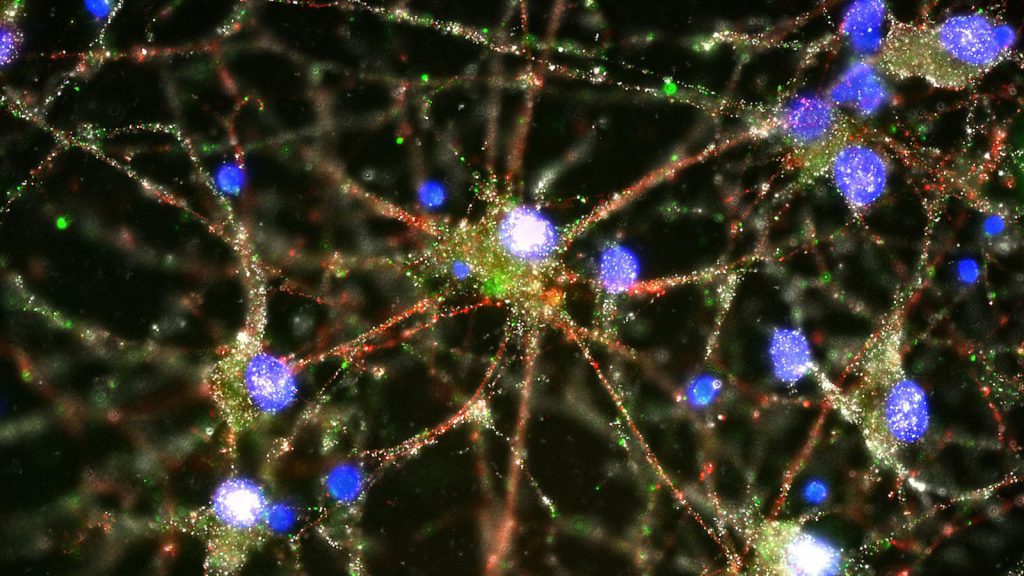
While studying such genetic defects might help scientists understand the neural pathways disrupted in some schizophrenia cases, it is far from certain that drug therapies could be designed that would selectively reverse such defects—especially if they arise during childhood, as the brain and nervous system develop, but are not detected until later. (Nearly all antipsychotic drugs on the market today target the neurotransmitter dopamine, which is known to be affected in schizophrenia. But critics of their use, or overuse, regard them as blunt instruments that dampen symptoms and do nothing to treat the underlying illness.)
In hopes of identifying more-common genes that could explain a greater number of schizophrenia cases, over the past decade researchers have turned to what are known as genome-wide association studies (GWAS)—scans of the genomes of tens of thousands of patients and controls. Yet while more than 100 genetic regions have been implicated in schizophrenia risk from GWAS so far, and hundreds more may be waiting to be found, none of them raise the risk more than a smidgen. One recent study, which identified an immune system gene called C4 that raises schizophrenia risk, found that the high-risk variant of that gene only increased the odds of a schizophrenia diagnosis from a baseline of 1 percent to 1.27 percent. Moreover, a closer look at the numbers in that study reveals the obstacles that genome researchers face in pinning down schizophrenia risk: While 27 percent of the nearly 29,000 schizophrenia patients in the study possessed the highest-risk variant of C4, some 22 percent of the 36,000-person control group also had that variant.
Genes are clearly important to understanding the disorder because researchers know from twin and family studies that some risk for schizophrenia is inherited. But the role genes play is much different than researchers had originally imagined, when they hoped the new genome technologies would unveil smoking gun genes of large effect. Instead, many researchers now think, the findings show that schizophrenia is highly “polygenic”—that is, many, many genes are involved, each contributing a small additional risk. That overall risk, in turn, may represent the biological substrate on which adverse life experiences wreak havoc for vulnerable people. Or, as Dillon puts it, “people have had bad things happen—that’s why they go mad.”
To some, relegating biological factors to a lesser role in schizophrenia causation might seem unjustified. People with psychotic symptoms are often profoundly and severely disturbed in ways that might suggest they are suffering from a brain disorder. Indeed, studies of schizophrenia patients often do show subtle differences in brain structure compared to healthy controls. But researchers debate whether such differences represent a cause or an effect of the underlying disorder. They may even indicate the effects of anti-psychotic drugs on the brain. And clinicians who work with patients stress that human psychology alone can play a tremendously powerful role in one’s experience of an illness. As anyone who has suffered from mental illness knows, experiencing these maladies can greatly disrupt one’s sense of being and self-worth.
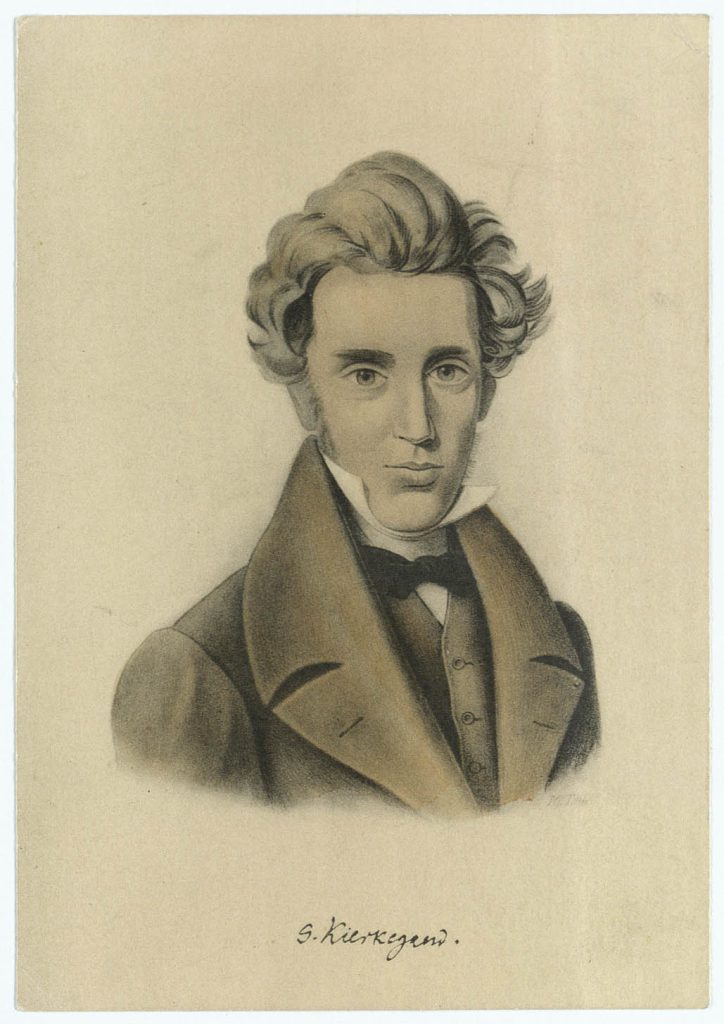
In the 19th century, this existential angst was vividly described by philosophers such as Søren Kierkegaard, who wrote about the “sickness unto death” caused by the anguish and despair of losing one’s self. Although he saw this human dilemma in religious terms—the sickness, he thought, was the result of being too far from God—his ideas inspired later existentialists. In the 20th century, psychoanalysts influenced by existentialism, including Rollo May and Erich Fromm, viewed the potential for mental illness as an integral part of the human condition.
More recently, some anthropologists and psychiatrists have argued that schizophrenia is a byproduct of modern human evolution and the cognitive complexities of our greatly enlarged brains, although such ideas are still very speculative.
Today some of the keenest insights into mental illness may be coming from anthropologists, who focus not only on the social, political, and economic context in which schizophrenia and related disorders arise, but the way that societies try to deal with them. “Anthropology holds up a mirror to biomedicine and how it is producing knowledge,” says Neely Laurenzo Myers, an anthropologist at Southern Methodist University in Dallas, Texas.
This mirror is the tool of ethnography—the descriptive study of living people and cultures. Some anthropologists, including Myers and Luhrmann (Myers’ former Ph.D. adviser), are using ethnographic inquiry to look at what is and is not working in the treatment of psychiatric patients. Myers, whose 2015 book Recovery’s Edge detailed her ethnographic study of a community program designed to help mentally ill patients recover, says that a key ingredient in recovery is “giving people a chance to create meaning around their experience.” In contrast, she says, most psychiatric treatment consists of heavily prescribed drugs that “dull the experience but are not helping people to do the deep mucking out of spiritual, emotional, and psychological work” that recovery requires.
These insights from anthropological research are also reflected in well-controlled epidemiological studies, which have consistently shown that social and economic factors can often increase the risk of schizophrenia more than any known genetic influences. These factors range from living in an urban rather than a rural environment to being an immigrant, living in poverty, emotional and sexual abuse (especially in childhood), and parental death, among others. In one meta-analysis—a review that combines many studies to increase their statistical power—published in 2012 in Schizophrenia Bulletin, researchers found that patients with psychosis were nearly three times as likely to have been victims of childhood adversity than healthy individuals in a control group.
Just why such social factors raise the risk of mental illness is still a matter of speculation, but many researchers suggest that they have one key feature in common: Such adversity raises the level of stress for people in those situations, sometimes to very high levels. People who carry a bit more genetic susceptibility into such situations could be more vulnerable—that is, they could more easily be tipped into full-blown psychosis.
Other investigations of the stress-vulnerability hypothesis examine the role that the stigma of being mentally ill plays in making symptoms of schizophrenia and other mental disorders even worse. The vicious cycle created when a diagnosed sufferer encounters negative reactions from other people can make recovery or remission all the more difficult. Recent work by clinical psychologist Victoria Vass of the University of Liverpool and her colleagues, for example, has revealed that a schizophrenia diagnosis in and of itself has a “highly damaging effect” on the ability to experience recovery, no matter how serious the symptoms actually are. And in a recent commentary in the BJPsych Bulletin, Paul Crichton, from the Ministry of Justice in the U.K., and his colleagues argued that psychiatric patients are particularly vulnerable to unjust treatment and prejudice, including by care workers and doctors themselves. The team singled out stigma and stereotyping as particularly problematic, pointing out that even physicians are sometimes guilty of such attitudes.
The complexities of these factors, however, should not lead researchers to abandon the search for relevant genes, even if the holy grail once sought by psychiatric geneticists is unlikely to be found. Regardless of whether the gene hunt leads to new drug therapies, understanding how genetic and environmental factors interact to produce an overall risk of schizophrenia and related disorders could help researchers identify those most vulnerable to falling ill, and perhaps allow mental health experts to intervene early enough, such as during a person’s childhood or early adolescence, to lessen or avoid serious symptoms.
And if it is indeed true, as many experts believe, that social factors and injustices such as poverty, racism, xenophobia, and child abuse are the greatest of all contributors to schizophrenia and related disorders, then all the more reason to attack them head on. As Dillon puts it, even if genes are playing an important role, “we need to make sure people’s environments don’t switch those things on. It doesn’t change what we need to do to stop people going mad.”
Of course, making such fundamental changes in our social fabric is a tall order, and it will take time. The deepest hopes of those seeking a more just society are unlikely to be realized in our lifetimes. Meanwhile, more funds are needed for both research and an expansion of personalized psychological approaches to treating schizophrenia, which have been shown to be modestly effective. These include both cognitive behavioral therapy (CBT) and more traditional psychoanalytic treatments. While such approaches are controversial—some critics have argued that there are significant flaws in studies that demonstrate their effectiveness—these treatments are well-established in Europe, especially in Scandinavian countries and the U.K. In Britain, health authorities officially recommend CBT for all first-episode cases of psychosis. And while such therapies may not reduce symptoms in all schizophrenia patients, they do have one crucial aspect: Psychological approaches treat patients as individual human beings whose suffering is worth all the time, effort, and money that society is capable of investing.
Broadening the use of such approaches might mean, in many cases, accepting that some symptoms typically seen as abnormal and psychotic actually play an important role in the lives of the people who have them. Although she still hears voices, Dillon says, “95 percent of them are positive now.” One of the most dominant voices, she adds, is that of a “great mother” figure who comforts and soothes her when she gets upset. “I don’t want my voices to be taken away,” she says, or blocked with antipsychotic drugs. “They are like a truth and reconciliation commission. The voices are coming to give evidence; they are trying to help me understand.”