Neighborliness Matters to Your Health

DOES GOOD HEALTH REQUIRE WEALTH?
The poorest people in the U.S. spend their lives sicker and die younger than the richest. Across Europe, people with low levels of education tend to live four to eight years less than the well-educated. A man born in a deprived neighborhood of Scotland can expect to experience poor health a staggering quarter century earlier than someone born in an affluent area.
In many industrial and post-industrial societies, the greater your wealth, the better your health.
Not so for Agta people living in the Philippines. In Agta society, individuals are considered wealthy if they own goggles and a speargun for fishing, and a pot to cook the catch. But poorer community members, who lack such amenities, do not necessarily suffer worse health.
As an anthropologist who researches health inequalities for a large humanitarian charity—and previously studied cooperation in various societies, including with the Agta—I have been exploring how a multiplicity of factors can lead to unfair but preventable differences in health.
Like other anthropologists, I’ve noticed that wealth has little bearing on health in numerous non-industrialized societies such as the Agta. Mounting evidence suggests why: The highly cooperative nature of these societies averts wealth-based health disparities.
If cultivated in culturally appropriate ways, this ethos of neighborliness could weaken health-wealth links where they exist in other communities. Some are already proving it.
WEALTH AMONG THE AGTA
Agta people live in luscious, forested mountains and on beaches along the northeastern coast of the Philippines. Traditionally, they lived in mobile, egalitarian groups. In such groups, wealth is readily shared. People regularly move from place to place to live with others. And social hierarchies are difficult to establish and maintain.
Over the past 20 years, some Agta people in the municipality of Palanan have settled in permanent villages and begun working for wages. They can more easily accrue radios, guns, cups, knives, and other useful items that also signify wealth. Thus, economic inequalities exist among village-dwellers.
To see whether this newfound wealth is impacting health, London School of Hygiene and Tropical Medicine anthropologist Abigail Page and colleagues lived with Agta people in Palanan over a two-year period. The researchers classified Agta communities as “mobile” if dwellings were simple lean-to shelters and people had relocated within the two years. “Settled” communities lived in wooden huts with metal roofs and access to infrastructure such as water pumps.
The team also asked Agta people to rank their possessions by importance, creating a locally meaningful list of assets. From these lists of who owns what, the researchers calculated wealth inequalities within each of the Agta communities.
Finally, the researchers surveyed people’s health by measuring blood pressure, red and white blood cell counts, and body mass index (BMI).
The results showed wealth inequalities existed in settled camps because people there could stockpile guns, cooking equipment, and other valuable items. But these inequalities did not translate into meaningful disparities in health.
The research team thinks this result was due to the cooperative nature of Agta society. Sharing and reciprocity are the norm, even while some accrue more goods. Although this study is a preprint undergoing peer review, the findings are striking: Wealth inequalities don’t inevitably lead to unfair differences in people’s health.
WHEN WEALTH DOESN’T PREDICT HEALTH
The findings from the recent Agta study build on evidence from other societies. Some studies of Tsimane forager-farmers in Bolivia showed that disparities in wealth did not affect self-rated health status, stress, depression, nutrition, or the risks of catching some infectious diseases. [1] [1] However, one of the studies found that poorer individuals showed some worse health measures, including higher blood pressure and more respiratory diseases.
For Turkana cattle herders in Kenya, there were no clear links between social standing and common causes of health inequalities such as stress or diet. And among Hadza hunter-gatherers in Tanzania, relative social standing—based on popularity and reputation as a good hunter—was not linked to stress, which is a common precipitator of poor health.
Living in different environments with distinct cultures, the Hadza, Turkana, Tsimane, Agta, and other non-industrialized societies share some common features. They maintain strong social support networks and feel obligations toward neighbors. Sharing is a key facet of everyday life, particularly when it comes to food. People do not have to disproportionately suffer just because they possess less wealth than others, and decisions are made collectively.
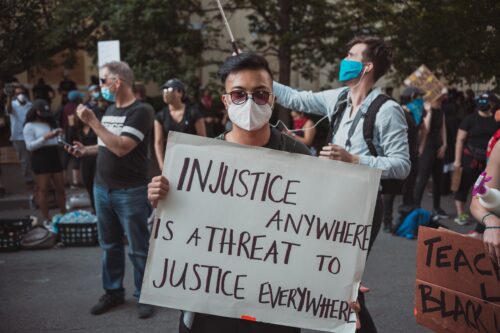
Meanwhile, in many large-scale, market-oriented, post-industrial nations, drastic health disparities exist and in many cases are worsening. Where I live, in the U.K., preventable inequalities in people’s health increased during the 2010s. Government cuts to public services have torn massive holes in the social security net. Austerity policies have caused an estimated 335,000 additional deaths over a seven-year period.
Similar patterns hold in other industrial and post-industrial societies. Poor health plagues people living in poverty, especially those in marginalized and minoritized groups. The wealthy amass power over others (by becoming part of an elite ruling class, for example), and this imbalance of power further entrenches health disparities.
NEIGHBORLINESS DAMPENS HEALTH DISPARITIES
Anthropological studies suggest ways societies with unfair health disparities could be reformed. One route, which I call neighborliness, entails looking out for and looking after others. Neighborliness is a nebulous concept, but I define it as an amalgam of trust, inclusion, sharing, reciprocity, redistribution, social cohesion, and civic engagement. In short, being kind to those around you and engaged in their lives.
In large-scale societies, neighborliness may seem complicated. After all, research suggests humans struggle to maintain more than a few hundred social relationships. Beyond that point, we need institutions such as a social security system to guide cooperation, enabling positive outcomes for as many people as possible. Essentially, people outsource neighborliness to the state.
But a touch more person-to-person neighborliness might help reduce unfair health disparities. Beyond patching holes in the social safety net, neighborliness can reveal ways to weave new, stronger safety nets. Sharing knowledge, experiences, and material goods can help our neighbors secure meaningful work, nutritious food, and adequate shelter. Biologically, neighborliness has been shown to alleviate chronic stress—a disease-causer that hits marginalized groups and people in vulnerable situations the hardest.
To be clear, this is not an argument to get rid of state welfare systems and instead rely on the kindness of strangers. Many populations are too large and their inequalities too entrenched. Larger welfare states, like those found in the Nordic countries, weaken the link between inequalities of health and economics.
It won’t be easy to create neighborliness at scale. Too many communities have been minoritized for so long, lack the resources to meet their essential needs, and face ongoing discrimination. All of this erodes the trust needed to look out for one another.
There will be no one-size-fits-all answer; trust looks different around the world and is shaped by social norms and expectations. But some places are already providing models of what neighborliness and meaningful inclusion could look like at various scales—from the national down to the hyper-local.
Movements like citizens’ assemblies have shown the power of inclusive, deliberative approaches to public policy decisions. In the Republic of Ireland, the Oireachtas (parliament) has set up several citizens’ assemblies over the past decade. Composed of members who reflect the wider population, these assemblies offer recommendations on sometimes controversial policy questions including abortion and same-sex marriage. For these two matters, integral to public health, the assemblies’ recommendations ultimately led the country to legalize both.
As another example, the city of Helsinki in Finland involved thousands of citizens in the design of its public library. But this is no ordinary library: Oodi acts as a community hub for millions of visitors a year, offering a warm and welcoming space to build connection and, in the words of its director, “break social bubbles.”
And on a smaller scale, a single street in suburban Western Australia transformed itself into a sustainable and inclusive community. On this street, residents do more than occupy the same space. They build things, share skills, grow and eat food together, and look out for vulnerable neighbors. Some residents literally pulled down the fences dividing them—creating a safe and healthy place to thrive.
Being kinder to one another and more willing to share may sound like glib solutions to the thorny issue of deep and persistent inequality. But as numerous communities and societies have already shown, kindness and sharing do help—whether we live on a Palanan beach or in a Palo Alto apartment.