How Natural Birth Became Inaccessible to the Poor

Pilar gave birth in a private, “humanized” hospital in Mexico City that takes a holistic approach to health and combines world-class medicine with the comforts of a five-star hotel. [1] [1] All names in this article, except for the author’s and Jan Tritten’s, have been changed to protect people’s privacy. The exterior walls of the hospital are covered with ivy, the floors are marble, and soothing tunes from a piano often echo in the multilevel foyer. Guests are served organic food. The bathrooms are appointed with terry cloth robes embroidered with the hospital’s emblem, and the tips of the toilet paper are carefully folded into a triangle. When I interviewed her, Pilar told me about her pleasant water birth in one of the hospital’s hot tubs.
But in a village that feels a world away from Pilar’s reality, Lupita’s birthing experience left a dark stain in her memory and pain in her heart. When she recognized that it was time to give birth, she sought the help of the village midwife, Leonila—an elderly woman who has used traditional techniques to bring children into the community for generations. Leonila had recently attended a government-mandated workshop where she and other midwives were informed about potential obstetric emergencies that can occur during the birthing process and instructed to refer all births to the regional hospital. So Lupita and her family loaded into a pickup truck, which trudged along a windy, uneven mountain path.
Leonila’s story of what happened next is shocking. By the time they arrived at the hospital, Lupita was on the brink of delivery. Her family clamored for the help of the hospital staff, but Lupita was refused service. When she could no longer hold the baby in, Lupita rushed into a bathroom and delivered a stillborn baby into the toilet bowl. A nurse burst in on the distraught, weeping Lupita and scolded her for the pool of blood. She ordered Lupita to clean up the mess.
While women in all countries have unique birth stories, in Mexico the appalling contrast between stories like those of Pilar and Lupita runs along deeply entrenched boundaries of race and class. Affluent, light-complexioned women enjoy humanized options provided by private care and accredited midwives, while poor Indigenous women are actively being deprived of access to the traditional birthing methods they have relied on for generations. Ironically, despite an increasing interest in natural birth in the country, traditional midwifery in Mexico is under siege.
From 2010 to 2014, I interviewed, spoke with, and observed more than 2,000 health professionals, hospital administrators, professors and instructors, medical anthropologists, fathers, and mothers all across Mexico. My informants included midwives, physicians, and more than 100 women undergoing pregnancy, birth, or the postpartum process. Their stories throw a spotlight on the shocking gap in Mexico’s birthing system between the country’s most vulnerable and most affluent women, which is where my work is situated.
In Mexico’s middle- and upper-class communities, high-tech births such as cesarean section are often the norm. According to Mexico’s National Survey of Health and Nutrition, 45.1 percent of all births in 2012 were via C-section—about quadruple the generally considered ideal rate of 10–15 percent. The World Health Organization has found that mortality rates for mothers and babies do not decrease when the cesarean rate is above about 10 percent, making it hard to justify the risk and expense of performing C-sections beyond this benchmark. Nonetheless, the rate of C-sections is even higher in Mexico’s private hospitals than in public clinics, indicating that middle- and upper-class Mexicans are actively seeking the procedure, even when not medically necessary.
It is in this context that thousands of fervent parents are passionately pursuing “humanized” births: natural birth (meaning without painkillers such as epidurals), home birth, water birth, and European-trained midwife- and doula-assisted birth. But these natural techniques are not cheap. In 2014, a midwife-assisted humanized birth package in Mexico City cost approximately 32,000 pesos (US$1,719 at today’s exchange rate)—1.3 years’ worth of earnings for someone making the minimum wage of 67 pesos per day, or about half the annual income of someone in the middle class.
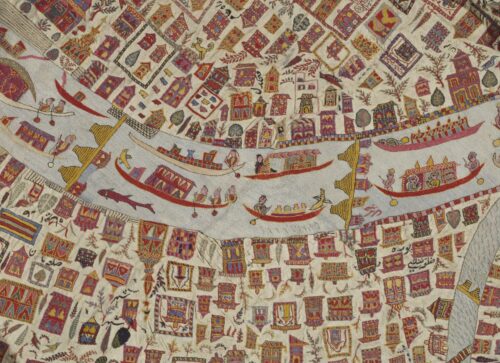
While many of the birth practices in humanized hospitals aim to “revive” the techniques of traditional midwives, ironically, traditional midwifery is being prohibited in many of the poor Indigenous communities where these techniques have endured for centuries. These birth techniques include massaging the pregnant woman’s belly to position the fetus, preparing herbal teas to stimulate the birthing process, various birthing postures that broaden the birth canal, ritual burying of the placenta near the home, and postpartum restoration through consuming bone broth and taking an herbal bath.
This threat against traditional midwifery practice has been institutionalized over the last decade: The government provides monthly stipends to the poorest quarter of the population conditional on their compliance with several rules, one of which is that pregnant women give birth in a government hospital. Traditional midwives like Leonila are required to direct all births to hospitals. And they are threatened with murder charges should a woman or baby die in their care, no matter how far they live from hospitals. Some of the women I met are several hours by bus or pickup truck from the nearest regional hospital where they are mandated to give birth.
These requirements might make sense if the quality of medical care was much higher in hospitals, as the government claims, or if traditional midwifery was resulting in particularly high levels of injury or death. But my research did not show either of these to be true. On the contrary, I found that women were too often receiving inferior care in hospitals, whereas I found the quality of care by midwives to be superior.
While the government blames midwifery practices for high maternal and infant mortality rates in Mexico’s most impoverished regions, I noticed that racial discrimination and insufficient infrastructure were recurring themes when interviewees recounted the deaths of wives, sisters, friends, and newborn children. People spoke of village clinics that are sporadically closed, chronically understaffed, and lacking in basic medications and instruments; crumbling roads that make emergency trips to the regional hospital extremely risky; and overcrowding at regional hospitals that leads to long wait times and forces women to lie in hallways on cardboard “cots” when all hospital beds are taken.
Given these dire conditions, many of the traditional midwives I interviewed feel that it is their ethical obligation to provide midwifery services to fellow villagers who seek their help. And while their interventions are in direct defiance of official government mandates, their actions are actually abetted by physicians in government posts who wish to wash their hands of potential responsibility for a maternal or infant death. At times, traditional midwives are directly encouraged to intervene: For example, a medical resident I talked to told me that he would rather refer a potential obstetric emergency to the local midwife than take the blame for whatever poor outcome might result. At other times, traditional midwives feel indirectly morally obligated to intercede in cases where medical staff fail to serve women: Another provider told me that his clinic will refer an obstetric emergency to the regional hospital knowing that the woman is likely to die in transit, since it is better that her death be logged as “in transit” than as having occurred in his clinic.
The Mexican government often uses traditional midwives as scapegoats; meanwhile, there are no official statistics on the birth outcomes of these midwives. The midwives I met had varied degrees of abilities and knowledge; some maintain private logs, which they keep secret from health officials, detailing thousands of successful births. The reputations of the most successful midwives, such as Eugenia, a renowned traditional midwife in the high mountains of Veracruz, are premised on empirical observations of their birth outcomes by villagers and clients from the surrounding region. They gain new clientele through word of mouth. Even one negative outcome can severely tarnish a midwife’s reputation. (This empirical, community-based form of ongoing validation runs counter to Western demands for statistical proof.)
The Mexican government often uses traditional midwives as scapegoats.
For many Indigenous women, being attended to by a trusted local midwife is the better option when compared to the possibility of having a tragic experience like Lupita’s.
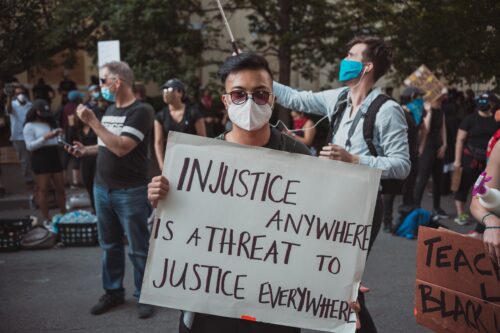
And their fear is understandable. Although it is illegal, some medical professionals at hospitals discriminate against their patients on the basis of “race”—it’s well-known that they sometimes do not treat Indigenous patients. Some cases, such as that of Irma—a Mazateca woman who was humiliated and forced to give birth in public on a hospital lawn—have been documented in major media outlets such as Proceso. And an upcoming report to the U.N. Human Rights Council outlines numerous human rights abuses against Indigenous peoples in Mexico. The death of Lupita’s baby signals her vulnerability on the basis of race and class, and her experience is not unique among people with the same set of vulnerabilities—for poor Indigenous women, the fear that discrimination can turn fatal is all too real.
Responses to this situation vary. Some traditional midwives and Indigenous women obey the government’s orders. Other Indigenous women begrudgingly attend their five government-mandated prenatal visits, with doctors who do not speak their language, while seeking obstetric care from a midwife on the side. (In 43 months of ethnographic research, I never once met a doctor who spoke the Indigenous language of the local population.) After giving birth with their midwives, these women would explain to health officials that the birth simply “came too fast” and they couldn’t make it to the hospital. Entire villages collude in this charade to skirt the system, which they feel is largely failing them.
Eugenia’s Nahuatl-speaking clientele drive up to 80 miles on winding mountain roads, from all around the Orizaba volcano, to give birth in her home clinic. Over the course of a few years, I earned the trust of Eugenia, and I watched her attend to both the obstetric and general health needs of the regional Indigenous population—which in one instance meant attending two births at once. After the births were over, Eugenia showed me how she records the details of the births she attends in a private log. While Eugenia used to accompany mothers to the hospital to request a birth certificate, she no longer does so, since the official story is that these women gave birth alone. If health officials found out about Eugenia’s full involvement, the new mothers could be stripped of their conditional cash transfers, and they would face even more extreme poverty. The village clinic is staffed by a medical intern who quietly supports Eugenia’s secret practice, since she relieves him of extra work in the face of limited infrastructure and medications.
There are programs that attempt to bridge the divide between traditional midwives and humanized birth practitioners. The accredited professional midwifery schools in Mexico require their students to give workshops to traditional midwives and to familiarize their traditional counterparts with Western biomedical standards.
The results can be somewhat absurd. Students in professional midwifery programs typically have very little experience attending births; theoretically, they participate in births at public hospitals—but obstetricians tend not to refer their patients away, preferring to keep insurance payments for treatment to themselves. (The majority of humanized births occur in the private sphere, since obstetricians in public hospitals do not attend humanized births. Therefore, public hospitals offer few opportunities for employment to professional midwives.) In contrast, many traditional midwives have thousands of births under their belts. During these student-led workshops, the traditional midwives often stare at the floor or wall in boredom, sometimes falling asleep, while being lectured to by less-experienced practitioners. Even with such “training,” traditional midwives still can’t openly practice.
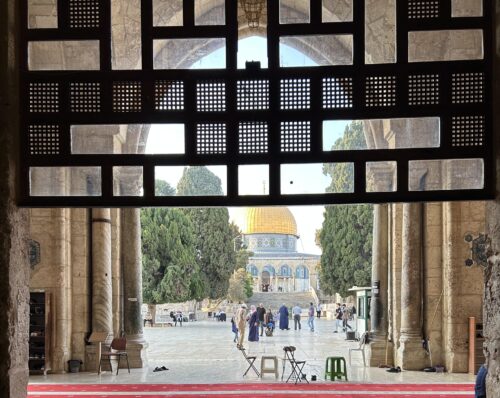
A few traditional midwives are proactive participants in the humanized birth movement. One such exception is Yanira, a traditional midwife I met in Tepoztlán in 2013. Yanira had happened to meet Jan Tritten, editor-in-chief of the Oregon-based magazine Midwifery Today. After that, Yanira began receiving a number of invitations to humanized birth conferences around the globe, including in Europe, Latin America, and the Middle East. However, Yanira has paid a heavy social price for her higher income and ability to travel internationally. She was forced to flee her hometown when jealous members of her community began to threaten her with kidnapping and demanded payments to leave her alone. She now practices with a much smaller clientele in a community of mostly European and American expatriates.
I am a proponent of birthing practices that respect women’s choices and resist the unnecessary hyper-medicalization of women’s bodies. However, humanized birth in Mexico should not be available only to wealthy, light-skinned people. Poor Indigenous people cannot access birth facilities like the one Pilar chose, of course. But they have birthing traditions of their own that stretch back thousands of years. The government’s attempts to control Indigenous women’s bodies are based on economic, cultural, and racial discrimination.
When Pilar checked out from her stay at the lush humanized hospital in Mexico City, she was given a wooden keepsake plaque with her baby’s footprints handcarved by an Indigenous artisan. This should not be the closest that Indigenous people come to natural birth.