Zika’s Frightening Stranglehold

Some of the earliest vampire stories were about demons or shape-shifters who spent their nights robbing pregnant women of their unborn fetuses, silently killing infants in their sleep, and sending children to an early grave. These stories embodied the fear and uncertainty surrounding miscarriages and the death of a child.
Although we now understand many of the underlying medical causes of these tragedies, the fundamental fear remains. Today that fear has a new face: the Zika virus. In South America, where a new strain of Zika has recently emerged with devastating health effects, increasing access to family planning will be a critical weapon in the fight against this new vampire.
Prior to 2015, Zika virus outbreaks had been isolated to certain areas of Africa, Southeast Asia, and the Pacific Islands. In May 2015, the first confirmed cases of Zika virus infection were reported in Brazil, and the Zika virus was tentatively linked to a frightening rise in neurological deficits in infants, including microcephaly, a condition characterized by abnormally small heads and limited brain growth. Children born with this condition may suffer related hearing and vision deficits, seizures, epilepsy, permanent brain damage, lifelong impairment, developmental delays, and early death. On March 31, 2016, the World Health Organization (WHO) announced that there is “strong scientific consensus” for a link between the Zika virus and various neurological disorders. Infected women are also at higher risk for miscarriages and stillbirths.
Earlier this year, in response to the growing crisis, the WHO had declared a public health emergency of international concern, recommending protective measures to reduce infections, especially among women of childbearing age and those already pregnant. Women are advised to guard against the mosquito that carries the virus by wearing long-sleeved shirts and pants, and by using mosquito bed nets, insect repellent, and window screens. In addition, people are encouraged to get rid of areas of standing water. Although practical, these recommendations can be challenging to follow in impoverished communities where daily food and shelter needs are often unmet.
Advice from the Brazilian, Colombian, Ecuadorean, and Salvadoran governments for women to avoid or delay pregnancy for the next two years comes as an additional burden.
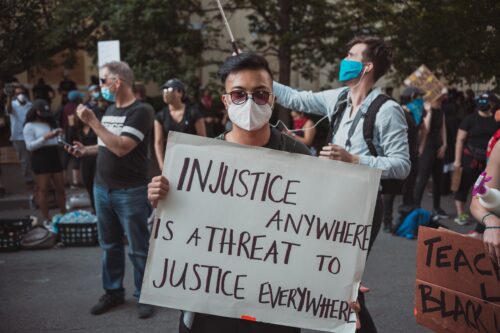
The logic is sound: Avoiding pregnancy is the best way to circumvent the severe birth defects associated with the Zika virus. But these recommendations ignore the extraordinary barriers women of reproductive age face and overlook the lack of educational, medical, and cultural infrastructure necessary for women to have the power to make family planning decisions.
At first blush, reproductive choice seems to be the sole responsibility of the individual. But the ability to make family planning decisions largely depends on cultural and social systems—religious, political, health care–related, educational, and legal—as well as cultural norms associated with family planning.
In the case of Latin America, the Roman Catholic Church has far-reaching influence over social systems as well as cultural norms. The Catholic Church has historically condemned artificial birth control; as a result, contraceptive use among Latin American women has been minimal—with family planning, in general, largely unavailable. The church’s doctrine has also influenced lawmakers. For instance, abortion—declared an “absolute evil” by the pope—is limited to cases of rape and maternal endangerment in the majority of South and Central American countries. In some countries, such as El Salvador, safe medical abortions are banned in all circumstances. The influence of the Catholic Church also extends to schools, where there is little reproductive-health education—or none at all. Not surprisingly, the average underage pregnancy rate in this region is more than 6 percent (compared to less than 3 percent in the United States). Among all Latin American women, more than half of pregnancies are unplanned.
Exacerbating this situation are the high levels of domestic and sexual abuse within these communities—more than a third of women report physical violence from an intimate partner or sexual abuse in their lifetime, compared to about a quarter in the United States. Most women in this region do not have the necessary legal and medical protections to safeguard themselves against their aggressors. In short, they lack control over their own sexuality and choices about any resulting pregnancies.
Today’s Zika crisis is not the first time that restrictions on family planning have resulted in tragedy for populations facing an infectious disease. The 1964 outbreak of rubella in the United States had catastrophic effects on families. Maternal infection during pregnancy led to the death of 2,100 newborns, and another 20,000 were born with complications similar to those caused by Zika, including microcephaly, blindness, and deafness. Although women were warned against getting pregnant at the time, the U.S. Supreme Court had yet to affirm their constitutional right to birth control or medical abortions. A high percentage of children who suffered from congenital rubella syndrome were institutionalized throughout their lives.
Zika’s rise has prompted an ethical reconsideration by the Catholic Church.
Fortunately, Zika’s rise has prompted an ethical reconsideration by the Catholic Church. There is a precedent for wiggle room in the church’s views on family planning: Pope Paul VI permitted nuns working in the Belgian Congo in the 1960s, who were at risk of wartime rape, to use birth control. In February 2016, Pope Francis hinted that the Catholic Church would condone birth control used to prevent pregnancies in areas affected by the Zika virus, saying, “avoiding pregnancy is not an absolute evil.” The Rev. Hector Figueroa, a Salvadoran priest charged with his nation’s health-related issues, has stated, “Morality says that people shouldn’t have that control [over family planning], but the church also isn’t going to say something that runs contrary to life and health.”
Although concessions from the Catholic Church are welcome, these statements alone are unlikely to have much impact in countries where hundreds of years of moral and religious doctrines have shaped family and social norms. Only when this advice is combined with increased access to birth control, safe medical abortions, and comprehensive reproductive education will women be empowered to follow the recommendations of their country.
When women in these populations are told to avoid pregnancy but are not provided with the necessary tools to comply, they run the risk of suffering the lifelong stigmatization and challenges associated with having and caring for a handicapped child. A complete response to this public health emergency requires an in-depth engagement with the cultural, sociopolitical, and historical systems that affect women’s access to family planning in Zika-affected regions worldwide.
Without addressing these barriers, we allow poverty, stigma, and the inaccessibility of comprehensive reproductive health care to create the same fear and uncertainty that vampires have been blamed for throughout history.