What Makes Injections Hard to Swallow?

If you’re watching a news show or reading a magazine article about vaccine hesitancy, you might find your program interspersed with advertisements for prescription medications: beguiling ads of cheerful, energetic people promising relief from everything from arthritis to late-stage cancer.
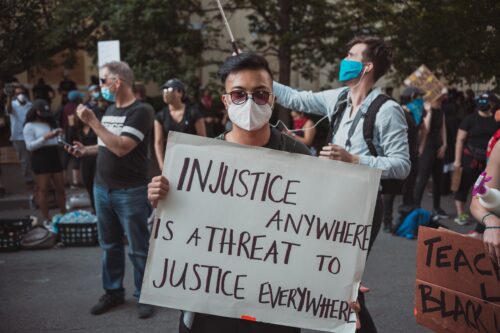
The juxtaposition seems completely illogical: How did some people develop a simultaneous rejection of certain medications and a whole-hearted zest for others?
As an archaeologist, I’m fascinated by the diversity of objects our ancestors have invented over millions of years, including those that people have used to introduce substances into their bodies. That includes culinary equipment associated with food production and the containers and accoutrements for medicines, enhancements, placebos, and recreational drugs. These objects have an intimate link to human perceptions of health and sickness—an essential part of our identity and daily routine, encompassed by the ubiquitous inquiry: “How are you?”
My work has led me to think about the human relationship with different mechanisms of medical delivery, particularly the pill and the injection. They differ in so many important ways: our level of independence in taking them, our level of comfort, and, importantly, the intended purpose of the drug for healing in the pressing present or protecting against a faraway future.
The human eagerness to take pills but a reluctance by some to be vaccinated surely has a lot to do with modern politics and social factors. But it also has roots deep in our ancestral past.
At this moment in history, as the planet undertakes a massive vaccination program, it seems ever-more important to understand these differences and to leverage lessons from the past as we move into the future.
The use of medicine has a very long history. Archaeologically, we know that the use of medicinal plants long preceded the development of domesticated plants. The knowledge of compounding goes back to the very earliest uses of writing, when recipes for both ingested and topical medications were some of the first things that scribes captured on clay, bamboo, and other surfaces.
A 3,600-year-old Egyptian papyrus, for example, provides “A Recipe for Transforming an Old Man Into a Youth.” The formula is quite complicated, involving large quantities of something called hemayet fruit that is bruised, dried, sifted, mixed with water, cooked, evaporated, and dried again, then rehydrated in river water, spread out to dry in the sun, and ground into a powder.
Ötzi the Copper Age traveler, whose frozen body was found in the Italian Alps in 1991, had in his kit bag two pieces of Piptoporus betulinus, a bracket fungus that has a flushing effect against intestinal parasites. (His autopsy revealed that he suffered from intestinal trouble—as most people probably did back then.)
While the practice of eating medicinal substances has likely been around for millions of years (even nonhuman primates self-medicate), injections are comparatively new. Projectiles such as spears and bullets have a long history of piercing the skin—but for purposes of harm.
Even after people developed invasive techniques to help rather than hurt, including acupuncture, amputation, and trepanation, there was still little experience of using violence to insert a compound into a person’s body with the counterintuitive goal of improving their health. Tattooing is one example: There is some evidence that millennia-old Indigenous tattoo practices were done in part to introduce therapeutic compounds. The idea of inoculating someone with traces of a disease to protect them seems to go back to before the 1500s in the Ottoman Empire. In Europe, the first vaccine was developed against smallpox in 1796. The first hypodermic syringe only dates to the 1850s.
Fear of needles may be as old as needles themselves and remains a problem even for those who require regular self-administered injections for their health, as with people who have diabetes.
Likewise, our long medicinal history was primarily focused on the ills of the here and now. While there is a relatively long history of preventive medicine stretching back thousands of years (for example, in China, India, and ancient Greece), our ancestors were surely more concerned with of-the-moment illness and injury than with future wellness. People well into the 19th century faced perpetual death and danger as very real wolves at the door. There was already plenty of pain and discomfort; the thought of adding more pain in the present to a healthy individual in order to forestall some possible future catastrophe would surely have made little sense.
A vaccine, counterintuitively, is taken when you’re well. You accept a physical pain (a pinch in the arm followed by side effects that can range from mild to severe) against an unknown future gain (a large statistical likelihood of protection against a deadly disease). This tradeoff means that vaccines join other things that are good for us that we don’t enjoy and often don’t do, like flossing or saving for retirement.
A vaccine, counterintuitively, is taken when you’re well.
Indeed, the challenges of imagining future benefits may be a critical part of the human story. Human cognitive misgivings surrounding pay-now/play-later activities are at the heart of many of our contemporary conundrums about health, economics, education, and climate change.
A final important distinction among medical applications is the notion of autonomy. Whether it’s swallowing a tablet, drinking a potion, or slapping a patch on your arm, the do-it-yourself approach seems to be popular: Hospital studies show that patients prefer to be in charge of their own medication.
By contrast, injections usually are given to you by a professional “other” who has special equipment and training; they are invasive procedures, done in commercial or institutional settings that may feel clinical and cold rather than comforting. It’s notable that when it comes to female hormonal birth control, pills are more popular than injections, even though the latter last longer and could enable people to avoid having to remember a daily pill.
Pills are perhaps the ultimate modern manifestation of the practice of self-treatment. As you take a pill, you can feel the effects of swallowing it and can often measure the impact in a matter of hours or less. Even if the effects are long-term or imperceptible, the psychological impact of taking a pill (even if it is a placebo) is significant. Drug manufacturers have learned to harness everything about pills, including their shape, size, and color, to produce the maximum desired effect. Advertisers know what they’re doing: They make people feel that by taking specific drugs, they’ll be just like the vibrant people they saw on TV.
The advent of what’s called “modern” medicine has arguably only been experienced within the last six human generations. It’s not surprising that our species is still coming to terms with narratives of health that involve preventive technologies delivered through invasive means.
But what if vaccines and other injections were reconceived in order to make the process more like taking pills?
Taste, visuals, and reformulated delivery mechanisms might be key elements to explore to make medicinal treatment more acceptable to deep-rooted human psychology. Small things can make a difference. The visual encouragement of vaccines, for example, is subtly encoded into Apple’s recently announced redesign of the syringe emoji to remove the potentially intimidating drops of blood that were part of the image.
Others are working to shift injected medicines, when possible, to other delivery systems in part to make them more acceptable. The typhoid vaccine is now widely available in a pill form; the seasonal flu vaccine can be administered as a nasal spray. Researchers have developed self-vaccination patches that have microneedles too small to feel; one survey suggested that the number of people willing to have a seasonal flu vaccine leapt from 46 percent to 65 percent with this technology. Researchers, including University of Pittsburgh bioengineer Emrullah Korkmaz, are already exploring this possibility for COVID-19 vaccines as well.
No doubt future medical treatments will continue to address our desire for autonomy in preventative and curative medicine, just as we cherish self-determination in other physical activities such as exercise, nutrition, and sex. With a little extra anthropological thought, we may well see a time when injections are part of the archaeology of medicine, with needles consigned to the dustbin of history.